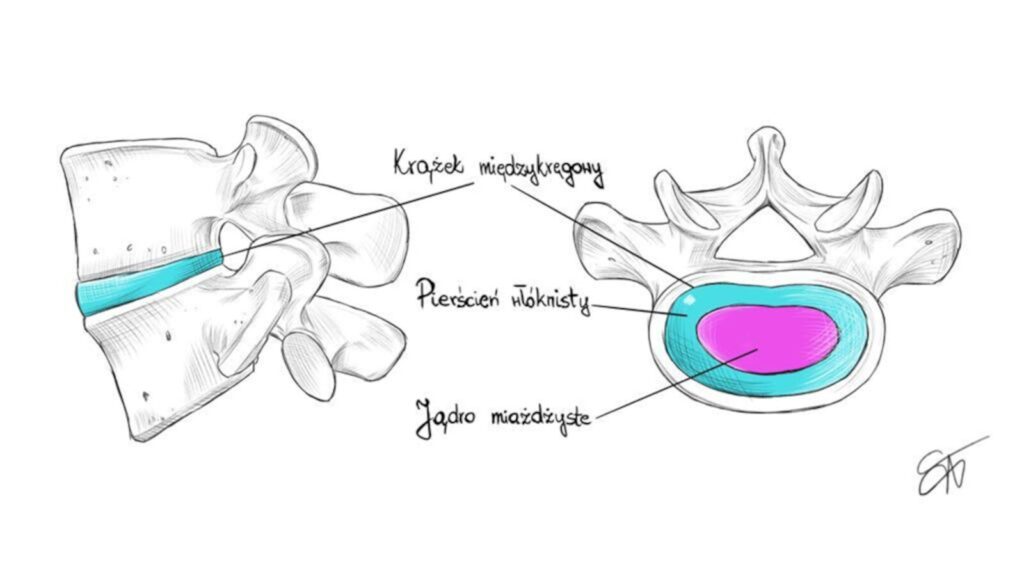
The intervertebral disc, commonly referred to simply as a "disc," is a structure located between two vertebral bodies of the spine and separated from them by a thin layer of cartilage called the endplate. The intervertebral disc itself consists of two components: the annulus fibrosus and the nucleus pulposus, also known as the gelatinous nucleus.
Pierścień włóknisty zbudowany jest z gęsto utkanych włókien kolagenowych zapewniających strukturze dysku odpowiednią sztywność. Jądro miażdżyste zbudowane jest natomiast głównie z wody , która w optymalnych warunkach stanowi około 90% jego zawartości. Poza wodą w skład jądra miażdżystego wchodzą nieliczne komórki, odpowiedzialne za wytwarzanie substancji wiążących cząsteczki wody wewnątrz jądra, zapewniając mu odpowiednią prężność. Dzięki temu działa ono jako amortyzator w kręgosłupie, rozkładając obciążenia i zapewniając elastyczność oraz odpowiednią ruchomość.
Discopathy is one of the most common spinal disorders, which can lead to chronic back pain and significant limitations in mobility. It primarily affects the lumbar spine, especially the L4-L5 and L5-S1 regions, as well as the cervical spine, which are subject to the greatest mechanical loads in daily life. As intervertebral discs degenerate, they become dehydrated, resulting in their shrinkage and loss of elasticity.Lumbar discopathy typically develops in individuals aged 30–50, and its causes include both the natural aging process and biomechanical factors as well as micro-injuries.
In this article, we will discuss the causes, diagnosis, treatment methods, and prevention of lumbar discopathy, which helps to avoid complications and improve patients’ quality of life.
Pathogenesis of Lumbar Discopathy
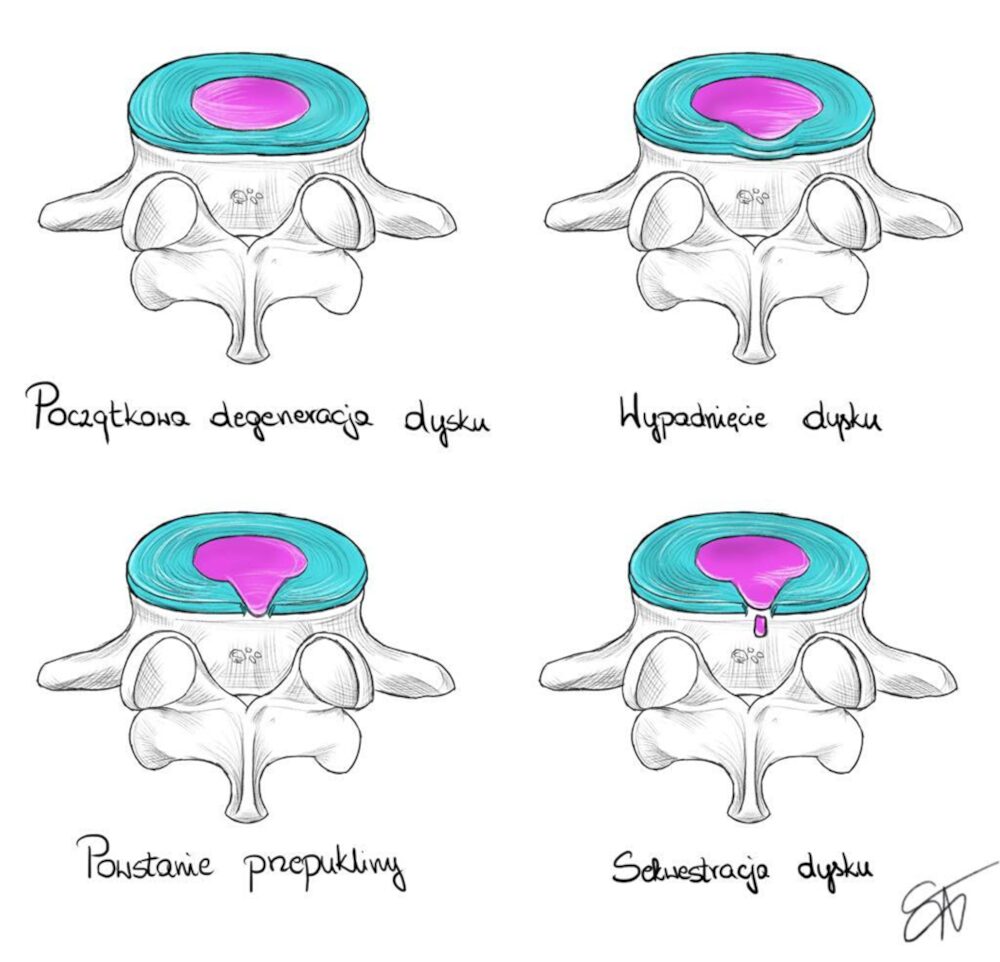
Lumbar discopathy is the result of degenerative processes occurring in the intervertebral discs. Due to dehydration of the nucleus pulposus, the disc height decreases and elasticity is lost, which affects the mechanics of individual spinal segments. As a result of these changes, the spine becomes more susceptible to micro-injuries and overload.
The main factors accelerating the development of lumbar discopathy include:
- Age With age, intervertebral discs lose water and proteoglycans, leading to weakening.
- Mechanical factors: Repetitive strain and lifting of heavy loads can accelerate degeneration.
- Poor Posture Prolonged strain on the lumbar spine, e.g., when sitting in an improper position, may intensify degenerative processes.
- Genetics: There are genetic predispositions to weaker intervertebral disc structure, which may increase the risk of discopathy.
- Lifestyle: Poor diet, smoking, and lack of physical activity also contribute to worsening the condition.s
Possibility of Herniated Disc Resorption
In cases where lumbar discopathy leads to a disc herniation, part of the disc material may protrude beyond the annulus fibrosus. However, in many cases, natural resorption (reabsorption) of the herniated tissue may occur. This phenomenon results from the body's inflammatory response, which mobilizes immune system cells to remove the damaged material.
Factors Supporting Disc Resorption:
- Sequestration: Detachment of a disc fragment from the main part facilitates its removal by the immune system.
- Inflammatory process: Increased activity of inflammatory mediators, such as macrophages, helps dissolve disc material.
Data shows that up to 70% of disc herniation cases undergo partial or complete resorption within 6–12 months of conservative treatment.
Diagnosis of Lumbar Discopathy
Accurate diagnosis of lumbar discopathy is based on a detailed clinical examination and appropriate imaging tests, which allow assessment of the condition of intervertebral discs and nerve structures.
Imaging tests::
- Magnetic Resonance Imaging (MRI): This is the gold standard in diagnosing lumbar discopathy. MRI allows assessment of structural changes in intervertebral discs, such as dehydration, reduced disc height, or damage to the annulus fibrosus.
- Spinal X-ray: Helps assess vertebral alignment and changes in intervertebral spaces, such as narrowing.
- Computed Tomography (CT): Used when bone changes are suspected, especially in advanced stages of discopathy.
- Neurological and Physiotherapeutic Assessment: Conducting a detailed neurological examination helps detect symptoms of nerve damage, such as sensory loss or mobility problems.
Conservative Treatment of Lumbar Discopathy
Conservative treatment is the first stage in the therapy of lumbar discopathy. The goal is to alleviate pain symptoms and improve spinal function without the need for surgical intervention.
Manual Therapies and Physiotherapy
- Manual therapy: Utilizes mobilization and manipulation techniques of joints and soft tissues, tool-assisted therapy, and needling techniques to reduce pain and accelerate the healing process.
- Physiotherapy: Regular exercises aimed at strengthening the paraspinal muscles and restoring spinal mobility in all physiological directions.
Pharmacotherapy
- Anti-inflammatory drugs:Recommended only for severe pain symptoms, as they may inhibit the natural process of disc resorption.
- Painkillers:Used to relieve symptoms in the short term.
Lifestyle Changes
- Workplace ergonomics: Adjusting working conditions to reduce spinal load. Regular breaks and proper positioning of chairs and desks are recommended.
- Physical activity: Regularne ćwiczenia poprawiające elastyczność i siłę mięśni przykręgosłupowych pomagają w zapobieganiu dalszym problemom z kręgosłupem.
Proper Diet: A diet rich in anti-inflammatory nutrients and adequate fluid intake supports the regeneration of intervertebral discs.
Surgical Treatment
Surgical treatment of lumbar discopathy is used only in cases where conservative treatment does not yield results or when there are serious neurological symptoms, such as nerve damage.
Indications for Surgery
- Cauda equina syndrome: A group of neurological symptoms requiring urgent surgical intervention.
- Progressive neurological deficits: Gradual loss of nerve function, such as muscle weakness or sensory disturbances. Stopniowa utrata funkcji nerwowych, takich jak osłabienie mięśni, zaburzenia czucia
- Persistent pain despite conservative treatment: When pain prevents normal daily functioning.
Surgical Procedures
- Microdiscectomy: Removal of the damaged portion of the disc to reduce pressure on the nerve root.
- Spinal stabilization: Use of implants to stabilize the damaged segment of the spine.
- Intervertebral disc prosthesis: In some cases, replacing the damaged disc with an artificial implant is considered, which helps restore spinal function.
Lumbar discopathy is a condition which, if left untreated, can negatively affect patients' quality of life. Early diagnosis, proper assessment, and the application of conservative treatment allow for effective symptom management and prevention of complicationss
Współpraca z doświadczonym fizjoterapeutą będzie właściwym rozwiązaniem zarówno w okresie ostrym jak i przewlekłym choroby dyskowej. Postępowanie powinno obejmować zarówno wdrożenie odpowiedniej terapii dla aktualnego okresu choroby, ale również zaplanowanie postępowania długoterminowego mającego na celu powrót do sprawności i funkcji społecznych.

Olga Okładło-Cygan
I am a physiotherapist, hirudotherapist and naturopath. I graduated from the Movement Rehabilitation Department of the Academy of Physical Education in Krakow in the field of Physiotherapy (2002-2007). Read more...
Check out the course
Ilustrował: Michał Składowski
Refrences
- PubMed 36722839
- PubMed 37559207
- PMC 4151413
- PubMed 11872180
- Orthopedic Reviews
- Chiro Trust: Herniated Disk Resorption